Last Updated: Aug 5, 2021
 By: Shyam Thakkar, MD
By: Shyam Thakkar, MD
The last few decades have been marked by tremendous advancements in endoscopic technology, which have redefined the practice of gastroenterology and gastrointestinal surgery. Looking back, however, endoscopic innovations were initially slow to start. The first fiberoptic endoscopy, performed in 1957 by Basil Hirschowitz, first down his own throat and a few days later down that of a patient, made remarkable progress in diminishing patient discomfort by enhancing flexibility and reducing bulk. From there, video endoscopy emerged, but it did not become mainstream until the mid-1980s. Since then, though, the endoscopic world has taken flight, with advancements so remarkable that essentially any procedure the mind can imagine can be performed.
Among the innumerable endoscopic innovations that have surfaced, Artificial Intelligence (AI), gives us the most comprehensive and complete path to the future. In its most basic form, AI is the theory and development of computer systems that can perform tasks that normally require the human brain, such as visual perception and decision-making. In recent years, the health care field has become a focus area of AI investment. In gastroenterology specifically, despite having numerous outstanding clinicians and health care providers, the quality of human performance can still fluctuate due to fatigue, interobserver variability, and lack of standardization. This is readily apparent and well-documented in screening colonoscopy. AI fills in these gaps as it has the potential to support human behavior, thereby reducing human burden while maintaining quality and reproducibility.
Endoscopy provides an outstanding platform for the application of AI. With image and data driven clinical algorithms, the adoption of AI is a natural progression in the field. Currently, AI developments in polyp detection, histologic analysis, report generation, and reduction of fluoroscopy are being studied. A centralized theme among these various AI technologies is the accurate and automated predictive capacity to accomplish the necessary task. This includes AI algorithms that function as a “second observer” to aid the endoscopist in identifying on-screen lesions, such as polyps or gastrointestinal bleeds (Fig 1). AI is also being tested for diagnostic purposes to classify polyp histology or delineate dysplasia in the setting of Barrett’s esophagus or inflammatory bowel disease during screening or surveillance exams (Fig 2). Our group has described the use of AI to measure exam quality in endoscopy by calculating the surface area and generating endoscopic thumbprints of the exams performed (Fig 3). Finally, through natural language processing, AI is being used for data extraction, with a prime example being calculation of adenoma detection rates. With this heightened activity, recent clinical trials have quickly moved AI to the forefront in gastroenterology. In fact, the first FDA-approved platform, GI Genius used for polyp detection with data supporting improvement in adenoma detection rates, is now commercially available. Over time, studies are likely to measure the impact of such systems themselves on the incidence of interval colorectal cancers.
Despite the rapid progression of AI technologies, significant barriers still remain. Understanding AI algorithms is a major concern among the physician community. Many raise worries over systems that are being developed without ways to understand how the algorithms are trained and validated. Even still, most will agree that AI is in our near future, and as expected, leading GI societies including the American Society for Gastrointestinal Endoscopy (ASGE) and World Endoscopy Organization (WEO) have developed task forces and committees focused on the healthy adoption of AI. These groups are expected to guide the infrastructure by which AI grows into the world of endoscopy. Over the next 5 years, we can likely expect educational symposia, enhanced fellowship training, rigorous assessments of research quality, guidance for AI trial design, and reimbursement support.
The opportunities for AI in gastroenterology, and specifically endoscopic gastroenterology, are boundless. As AI systems continue to expand their library of clinical applications and begin to have real-world applicability, the potential for improvement in procedural efficiency and accuracy could be dramatic. While clinician supervision of AI models will be necessary, it is paramount that physicians do not become dependent on AI, but rather leverage it to enhance the field and elevate patient care.
One of the presidential initiatives of Pennsylvania Medical Society (PAMED) President Michael DellaVecchia, MD, PhD, FACS, FICS, FCPP, is to prepare physicians for the advanced technologies such as AI, robotics, nanotechnology, and biosensors that will forever change medical education and the practice of medicine. As part of this initiative, Dr. DellaVecchia is hosting several interviews with national experts in these technologies. PAMED members can learn more on the PAMED website at http://www.pamedsoc.org/AI.
Fig 1. Polyp detection AI algorithm placing a boundary box around a subtle polyp. (Berzin, Tyler M., and Eric J. Topol. "Adding artificial intelligence to gastrointestinal endoscopy." The Lancet 395, no. 10223 (2020): 485.)
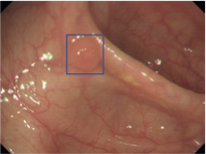
Fig 2. Polyp differentiation AI algorithm predicts adenomatous pathology of detected polyp (Kudo, Shin‐ei, Yuichi Mori, Masashi Misawa, Kenichi Takeda, Toyoki Kudo, Hayato Itoh, Masahiro Oda, and Kensaku Mori. "Artificial intelligence and colonoscopy: Current status and future perspectives." Digestive Endoscopy 31, no. 4 (2019): 363-371.)
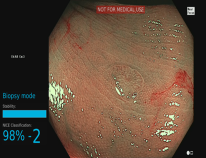
Fig 3. AI algorithm heat map demonstrating quality metrics of surface area, image clarity, colonic distention, and preparation over the course of an exam (Thakkar, Shyam, Neil M. Carleton, Bharat Rao, and Aslam Syed. "Use of artificial intelligence-based analytics from live colonoscopies to optimize the quality of the colonoscopy examination in real time: proof of concept." Gastroenterology158, no. 5 (2020): 1219-1221.)